
The patient journey
Placing patient experience at the forefront, our objective is to develop innovations that effectively address the specific challenges and needs faced by patients during their cancer care journey. This entails designing interventions that alleviate psychological and emotional burdens, enhance physical comfort, and improve overall well-being. We also recognise the significance of supporting healthcare workers by considering their perspectives, workflows, and integrating technologies that enhance their capabilities and streamline their practices.
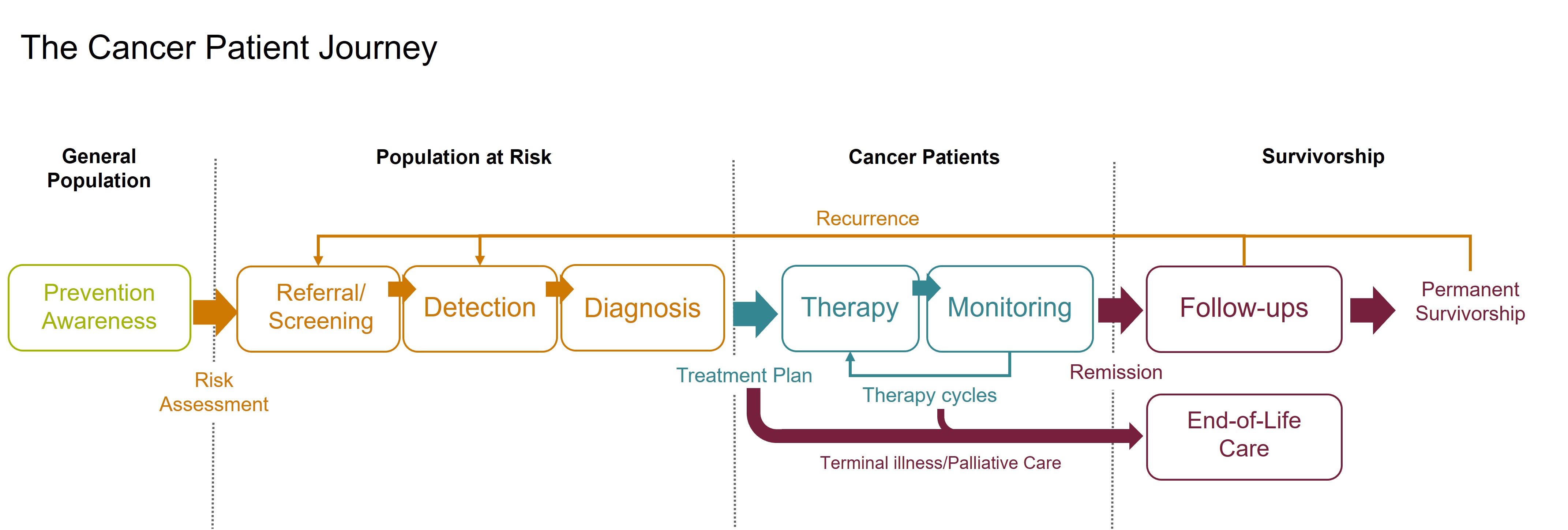

Improving cancer survival rates substantially relies on the timely diagnosis and treatment of the disease, particularly when aiming for a complete cure. Our focus on early detection encompasses two main areas: cancer metabolism biomarkers and the development of ultrasensitive detection technologies. Efforts in early detection focus on utilising risk-stratified populations to investigate the potential of biomarkers. We harness technological innovation by developing ultrasensitive low-cost devices to detect specific early disease signals, supported by clinical positioning and adoption strategies. The NHS Long Term Plan has expanded its ambitious plan to see an extra 55,000 people each year surviving for five years or more following their cancer diagnosis, and three in four cancers (75%) diagnosed at an early stage by 2028. In collaboration with our partner, we aspire to contribute to achieving this goal by proposing innovative solutions for early cancer detection and earlier diagnosis.
Surgery remains the most important curative option for most cancers. We develop techniques and technologies that improve surgical precision and advance surgical boundaries beyond the current standard of care. In radiotherapy, we build on expertise across multiple tumour indications to drive innovations leading to treatments that can be delivered with increased precision, over shorter fractionation schedules, and using functional image-guidance. Surgical and radiotherapy will be complemented by other interventional technologies. We exploit novel approaches to determine the exact extent of the tumour, based on physical and metabolic characterisation and radiological/radiomic and molecular imaging, to permit precise removal of malignant tissue and preservation of uninvolved normal tissue. We also study the potential for directing intra-tumour therapies to mediate both loco-regional and systemic effects, as stand-alone treatments and components of combination regimens.


Despite the vast array of therapies to treat cancer, a significant limitation of current treatment approaches is the ability to understand how well a patient is responding to their treatment. Typically, a patient will undergo blood tests and routine imaging scans to determine whether their treatment is working. These currently have significant limitations in terms of cost, impact on patients' lives, and efficacy – providing only an indication of the patient's status at that snapshot in time, and measuring relatively crude tumour-specific markers in terms of underlying biological response. Key challenges for the clinician are to understand how well the therapy is working and how to make decisions to change or stop therapy. Novel methods are needed to understand mechanisms of action and resistance of treatment with innovative assays to be able to predict response and resistance to treatment at the point of diagnosis. The goal is to develop low-cost therapy monitoring technologies that provide a real-time readout of therapeutic response, which can be implemented in a healthcare setting to inform treatment decision making.