Clinical development
Our ambition is to integrate convergence science technologies and framework into the widely adopted ICR-developed Pharmacological Audit Trail (integrated PhAT or iPhAT) to enable personalised cancer discovery research, focusing on tumour-specific vulnerabilities and mechanisms of resistance. Using the iPhAT clinical trial framework, we wish to ensure reiterative translational research between laboratory and clinical trials. The Clinical Development initiative is intrinsically connected to the Convergence Discovery Research theme to support reiterative bedside-to-bench therapeutic and discovery research to generate patient-derived cancer organoid models from trial patients and understand mechanisms of action and resistance. The Clinical Development initiative also supports the Interventional Science theme, by conducting trials that provide both ‘Proof of mechanism and ‘Proof of Concept’, demonstrating safety, tolerability and anti-tumour activity in stratified populations leading to rapid drug and device approval. We will continue to test innovative treatment combinations, with emphasis on immuno-oncology agents in combination with targeted therapies or with radiation therapy in a range of tumour types.

To maximise the likelihood of progressing promising clinical candidates through early phase trials, we employ a range of convergence science approaches to facilitate both forward and reverse translation to refine and test clinical hypotheses. The ICR/RMH Drug Development Unit (DDU), is a world leader in the design and conduct of early clinical and translational studies, committed to the rapid and successful transition of novel agents into registration trials to accelerate their approval. The centre wants to support clinical trials testing convergence science therapeutics or modes of delivery, and using convergence science technologies to optimise treatments and understand therapy resistance.
Our Centre prioritise close interdigitation of clinical trials with studies of corresponding relevant preclinical models. Explant cultures have significant promise for the study of therapeutic response but are currently limited to very short-term culturing. We are developing engineered devices that promote longer-term explant culture to develop predictive models for patient response. Human cancer organoids were shown to be good predictors of the patient treatment responses, and we routinely establish patient-derived cancer organoid for post-clinical biochemical and pharmacological analyses in parallel with ongoing human phase I/II clinical trials, enabling personalised cancer discovery research, focusing on optimisation of patient treatments, tumour-specific vulnerabilities, and mechanisms of resistance.

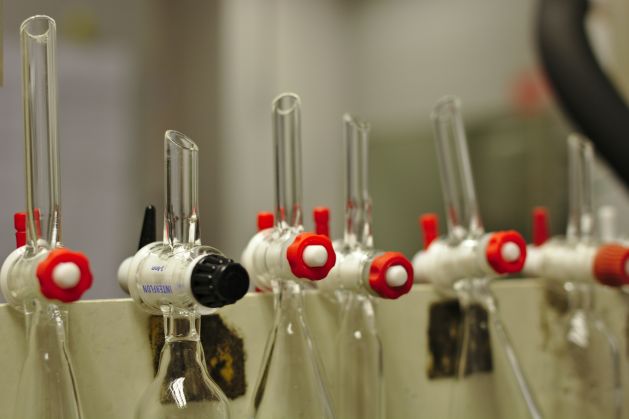
A common feature of most small molecule drugs is that their persistent mode of action, either permanently inhibiting or activating their targets. As a result, these drugs elicit compensatory responses leading to tolerance or resistance over time. Novel chemistry- and biological-based therapeutic approaches that complement conventional drug discovery are needed to develop milder therapies that support extended treatment regimes to manage cancer in the longer term. Traditional small molecule drug discovery for cancer therapy has a high failure rate. This is often linked to limitations of screening readouts and/or the model systems used. The development of new drug screening methodologies using more biologically relevant systems is urgently required.